MONTREAL - Everyone knows there are not enough doctors in Quebec.
More than two million Quebecers are without a family physician, a number that has only grown since the mid-1990s.
Since then the province has been playing catch-up, and finding it difficult to convince young doctors to focus on family medicine, or to treat patients in rural areas.
Anglophones seeking medical care in their own language also face challenges.
Last year Pat Bigney was one of several hundred patients suddenly orphaned by the medical system when their West Island physician decided it was time to stop working.
"Unfortunately he decided to retire and that was it! He did try to find somebody to take over his practice and was unable," said Bigney.
After a year of searching, despite her good health, she has been unable to find a replacement for the man who looked after her for two decades.
No anglophone doctors on Montreal's West Island are openly accepting patients.
"I've been looking around. I've been asking everybody I know and there just aren't any family physicians that have openings," said Bigney.
"The system is, if I may, kind of broken at this point."
Patients turning to clinics
Without a family doctor, millions of Quebecers rely on clinics to provide primary care, but the lack of consistency in care can create more problems.
Eleanor Phelan Mootoosawmy of the Statcare Medical Clinic sees the casualties of the broken system every day.
Her walk-in clinic is open seven days a week, and has a near-constant lineup outside.
"In the morning you can have a lineup of 50-60 patients waiting prior to the doors opening at 7:30," said Mootoosawmy.
For the most part patients have nowhere else to go and are no longer even trying to find a primary care physician.
"I would say percent of our patients do not have a family doctor," said Mootoosawmy. "A lot of the elderly patients have given up."
Young doctors not interested
Dr. Jeannette Janzen moved to Quebec from Saskatchewan 50 years ago, and she warns the lack of family doctors will have consequences.
"With diabetes, with MS, with new cancers, [all are] very serious diseases which actually need good follow-up," said Dr. Janzen.
As the population ages and people come down with so-called "first-world diseases," Janzen says people will need the consistent care that can only be provided by regular contact with a family physician familiar with a patient's history.
"Neglect I call it," he said. "It's really third world."
Janzen works in a clinic, and she does not see young doctors eager to take her place.
"We have a lot of doctors [who are] 55-60-65, ready to retire. Where are the 40-year-olds and where are the 30-year-olds? They're not around," he said.
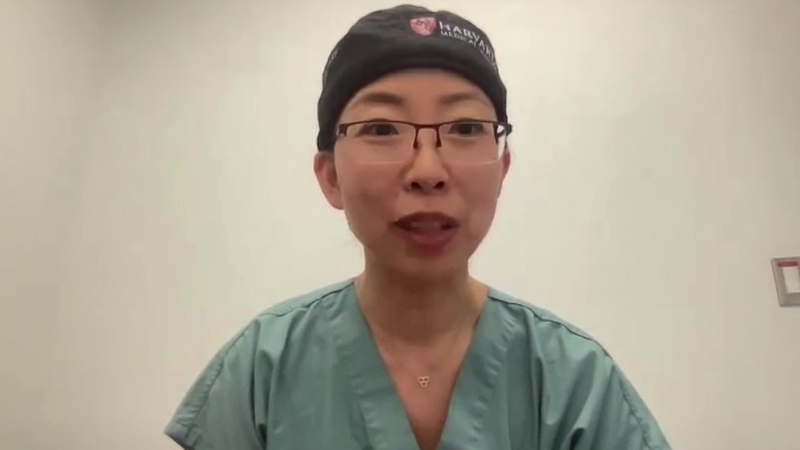
Dr. Irene Simons, who began practicing in Quebec 42 years ago, is still seeing about 60 patients a day between her private practice and a walk-in clinic.
She worries about a coming tsunami of aging people with complex health problems swamping a decreasing number of older doctors like herself.
Eligible for retirement, she'd like to cut back but doesn't feel she can.
"Right now I feel like I'm a fireman putting out fires," said Dr. Simons.
When she does stop practicing, she knows her 1800 patients will be frustrated and angry.
"I think the only accepted way to leave the practice of medicine seems to be to die. Because if you die, the patients can't get too angry."
The carrot-and-stick approach, without a carrot
Many people say the medical crisis began in the mid-1990s when the Parti Quebecois government offered early retirement to physicians and a larger-than-expected number decided to end their careers.
At the same time as thousands of doctors hung up their stethoscopes, the government cut the number of spaces in the province's medical schools.
It also imposed a number of disincentives for young family doctors.
Recent medical school graduates have to work in rural regions or take a financial hit. They have to dedicate 20 years to working in clinics and hospitals instead of being allowed to work only in a private practice.
After nearly two decades of what many call mismanagement, the average age of a GP in Quebec is 51 years old, and young doctors, more than ever, are leaving the province.
No one knows this better than the head of the Jewish General Hospital's Family Medicine Programme.
Dr. Michael Malus's own son trained in Quebec to become a doctor, then left to practice medicine elsewhere.
"It's painfully frustrating, because we'd like them to be able to to be taking care of people out there in Montreal who 40 percent don't have a family doctor.
The Jewish General offers two-year residencies to young doctors, only to see many of them leave to get paid more elsewhere.
"It's not really competitive by normal North American standards and we're losing these doctors," said Dr. Malus
The latest disincentive happened in December 2010, when the provincial government stopped communicating with doctors in English.
"Everything comes only in French and they will not deal with us in English," said Dr. Simons. "How are we going to get doctors from outside the province if they won't communicate with them?"
Another problem is the lower pay associated with being a general practitioner.
With fees dictated by the provincial government, specialists can earn more money.
Dr. Marc-Andre Asselin of the Quebec Federation of GP's says residents are choosing to pursue more education.
"In the last five years, 260 places in family medicine, in residency hasn't been taken by the residents. They're all going in specialties," said Dr. Asselin.
The federation is now negotiating a new contract demanding better working conditions and salary increases.
Change in the offing
The province's health minister is himself a doctor, and Yves Bolduc says improving access is a key concern for the government.
"We should have more doctors, but also have a better organization," said Bolduc.
General Practitioners say change has to come fast, and it has to work.
"It totally worries me," said Dr. Simons. "I don't know who's going to look after me when I'm old. I know doctors who can't find doctors."
The problem does show signs of being fixed.
The College of Physicians added 430 doctors to its ranks in 2010, which is the largest increase in 15 years.
Bolduc also just announced 237 new specialist positions, 57 percent of which will be in the province's rural areas.
However while spaces are being added in medical schools, there are no guarantees that doctors will stay once they graduate.